The original version of this post ran June 2016. I’ve added an update to the end.
In 2001, Dean Spath was diagnosed with advanced prostate cancer. He had surgery to remove his prostate, and for nearly a decade, Spath appeared to be cancer free. Each year he would visit the doctor to have a blood test and a scan, and each year the tests came back clean. “They thought they got it all,” Spath says. “I was hoping I was cured.” In January 2011, however, a blood test revealed that Spath’s PSA level, a marker of disease progression, was on the rise. By June a malignant spot had appeared on his rib. The cancer was back.
First, Spath underwent eight weeks of radiation. And then he began receiving an injection to suppress testosterone, a hormone that fuels prostate cancer. Next he tried a new kind of immune therapy. But no matter what Spath’s physicians gave him, they couldn’t eradicate the cancer.
Spath is far from alone. All over the world, people with metastatic cancer are fighting a losing battle. Even when oncologists use the most targeted, cutting-edge therapies, patients develop resistance and their cancer comes thundering back.
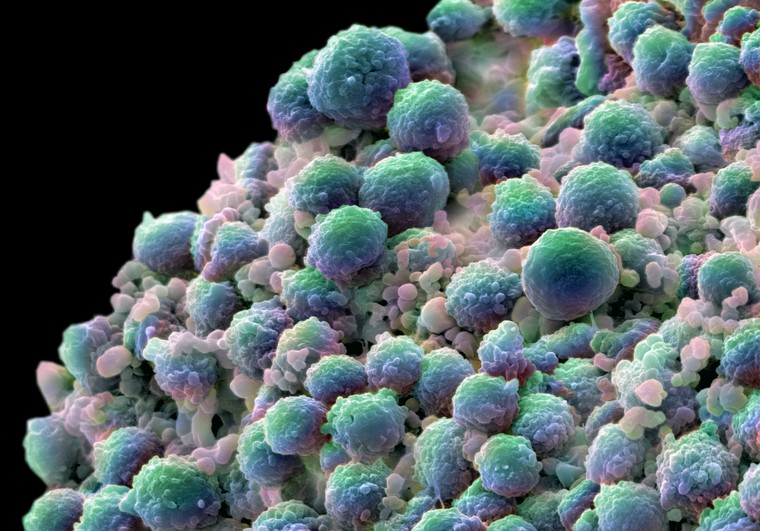
The problem is that cancer is so monumentally diverse. Tumors begin as a single cell that keeps dividing. The daughters should be perfect clones, but some pick up genetic defects that make them distinct. This genetic diversity allows the tumor to evolve. Resistance is inevitable, says Bert Vogelstein, a cancer geneticist at Johns Hopkins University in Baltimore. “All of the mutations that are responsible for resistance are already present in each metastatic lesion before any treatment is begun,” he says. “It’s a fait accompli.”
But Robert Gatenby, a molecular oncologist at Moffitt Cancer Center in Tampa, Florida, thinks he may have a fix. What if we lower the bar? Instead of trying to cure individuals with incurable cancer, what if we help them live with their disease? Could we stave off resistance and buy more time?
Gatenby points out that oncologists are trained to go in with guns blazing, aiming to kill as many cancer cells as possible. “It is simply assumed that this is the right approach,” he says. But think about it from an ecological perspective, and the strategy doesn’t make sense for patients who have advanced cancers. Resistance already lurks within the tumor’s diversity. Killing all the drug-susceptible cancer cells only leaves a bonanza of resources for the drug-resistant cells. More drugs breed more resistance, and eventually the cancer becomes unstoppable.
“We torture patients, in a sense,” says Darryl Shibata, a pathologist at the University of Southern California. “All we do is make their tumor really aggressive, and it kills them.”
Gatenby is trying a gentler approach — adaptive therapy. He hopes to keep cancer from progressing by carefully changing the dose or timing of therapy depending on the tumor’s response. The goal is to control the disease rather than eliminate it. This may seem like a radical idea to a country used to thinking about cancer as a “war” that we “fight” with an anti-cancer “arsenal.” But this adaptive approach has been standard practice in pest management since the 1970s, when researchers realized that the widespread use of insecticides quickly selected for resistant insects. In fact, in 1972, President Nixon made integrated pest management — a strategy that emphasizes control over eradication — national policy. “The same administration which gave us the war on cancer and that kind of war-like language that dominates our thinking about it adopted a much more subtle approach to pest management,” Gatenby says.
Studies suggest adaptive therapy can work in mice, and last year researchers at Moffitt Cancer Center launched a clinical trial to test whether adaptive therapy can work in humans. Spath is one of the first test cases.
Spath and the other study participants receive Zytiga, a therapy that stops the production of testosterone. Most men with prostate cancer take Zytiga continuously, but in this study the subjects start and stop the drug depending on their tumor’s response. Each participant receives a monthly blood test to check his PSA level. If the level falls by 50% or more from baseline, he stops taking the drug. If it rises 50% or more, he starts taking the drug again. “The goal is to maintain a population of sensitive cells that will suppress the growth of the resistant cells,” Gatenby says. “We want to use the cells that we can control to suppress the growth of the cells that we can’t control.”
Spath can’t explain the nuances of adaptive therapy, but he knows that, for the moment at least, Gatenby’s strategy seems to be working. Spath has already lost two friends to prostate cancer, and both received their diagnoses after he did. “I’m living on borrowed time,” he says. But he and his wife, Barbara, don’t spend much time worrying about it. The years have tempered their fear of the disease. “We’re going to live life to the fullest until we can’t any longer,” says Spath’s wife, Barbara. “We all have an expiration date. None of us knows when it is.”
Spath’s time ran out October 1, 2018. He died at home with Barbara and the rest of his family by his side.
You can find a much longer article I wrote on cancer and evolution for Nature in 2016 here. Roxanne Khamsi also wrote an excellent feature about Gatenby for the April issue of Wired.
***
Image of prostate cancer cells by Annie Cavanagh. Wellcome Image Awards 2008.
“Health statistics represent people with the tears wiped off.”