Influenza hit the US hard this winter. In December, the Centers for Disease Control and Prevention (CDC) reported that influenza had reached epidemic proportions across large swaths of the country. Most of us think of the flu as an inconvenience, but the virus can be deadly. In early January, a 26-year-old radiology technician in Wisconsin died when her illness morphed into a blood infection that stopped her heart.
The best way to protect yourself from infection is the flu vaccine. But the shot doesn’t always work. In good years, the flu vaccine is only about 60% effective. And this year is not a good year. Last week the CDC reported that the current vaccine appears to have an effectiveness of just 23%. That means that this season’s vaccine cuts the risk of a doctor’s visit for flu symptoms by about 23%. The vaccine is even less effective in adults and seniors.
To understand why this year’s shot is so ineffective, you first need to know a little something about influenza. The flu isn’t caused by one virus, it’s caused by many. There are three species of influenza, and the most common species is broken into different subtypes. To classify these subtypes, scientists use two proteins found on the surface of the virus: hemagglutinin (H) and neuraminidase (N). That’s why you see the flu referred to as H3N2, or H1N1. But the viruses are constantly evolving in an attempt to stay one step ahead of our immune system, and even within subtypes there’s wild variety. That’s why getting the flu doesn’t prevent you from getting it again. And that’s why last year’s vaccine doesn’t typically protect you from this year’s flu.
 To make an effective vaccine, researchers rely on year-round surveillance from more than 140 influenza centers in 111 countries. These centers then send viruses to a handful of top-tier labs that collaborate with the World Health Organization (WHO). Based on this info, the World Health Organization issues a formal recommendation twice a year about which strains should be included in the flu vaccine. These announcements give vaccine manufacturers six to eight months to churn out millions of doses of vaccine before the flu season hits in the Northern and Southern hemispheres.
To make an effective vaccine, researchers rely on year-round surveillance from more than 140 influenza centers in 111 countries. These centers then send viruses to a handful of top-tier labs that collaborate with the World Health Organization (WHO). Based on this info, the World Health Organization issues a formal recommendation twice a year about which strains should be included in the flu vaccine. These announcements give vaccine manufacturers six to eight months to churn out millions of doses of vaccine before the flu season hits in the Northern and Southern hemispheres.
But predicting which flu strains will be circulating months in advance is a tricky business, and WHO’s forecast doesn’t always pan out. In February 2014, WHO recommended that the flu vaccine in the Northern hemisphere contain a strain of H3N2 collected in Texas in 2012. But about a month later a slightly different strain of H3N2 emerged. Only a small number of these viruses were circulating at the time, but by December, this altered H3N2 had become one of the dominant strains. In January, the CDC reported that 65% of the 349 H3N2 viruses tested thus far were a poor match for the H3N2 vaccine strain.
Like many vaccines, the flu vaccine works by prompting the immune system to make antibodies. These antibodies help stave off infection when you encounter the wild virus. But antibodies against one strain of influenza don’t necessarily work against other strains, even ones that are closely related. And there’s the rub. If WHO makes a bad prediction, the vaccine’s effectiveness can plummet.
By now I’ve no doubt convinced you that this year’s flu shot doesn’t work very well. So why get vaccinated? I’ll give you four reasons.
–First, because some protection is better than none. Influenza is rampant this year, and you have no way of knowing which strain of the flu you might run into. The vaccine protects against three (or four) strains, and only one appears to be a bad match.
–If the shot does stop you from catching the flu, it will also stop you from spreading it. And your spouse, children, and coworkers will thank you.
–The vaccine is safe, and the most common side effects— soreness, redness, tenderness or swelling—are mild.
–Even when the virus that’s circulating doesn’t match the vaccine virus, the shot might provide some protection against severe illness. For example, the flu might still force you to spend several days moaning under the covers, but perhaps the vaccine will help you skip the hospital stay.
According to a CDC survey, just 40% of children and adults had been vaccinated as of November 2014. What are the other 60% of you waiting for?
***
Image credit top: Corpsmen in cap and gown ready to attend patients in influenza ward in 1918. Courtesy of Wikimedia Commons

Only 40%? Wow. I assumed it was higher.
Speaking of not vaccinating. Check out this LA Times graphic on vaccination rates at nearly a thousand California elementary schools. http://spreadsheets.latimes.com/immunization-levels-california/ At many schools, 25% to 75% of kindergarteners haven’t been vaccinated. The worst seem to be private schools like Waldorf. Some areas, like my home town of Santa Cruz, are hot beds of antivaxxers. There’s hardly any herd immunity anywhere among school kids between Sacramento and the Oregon border.
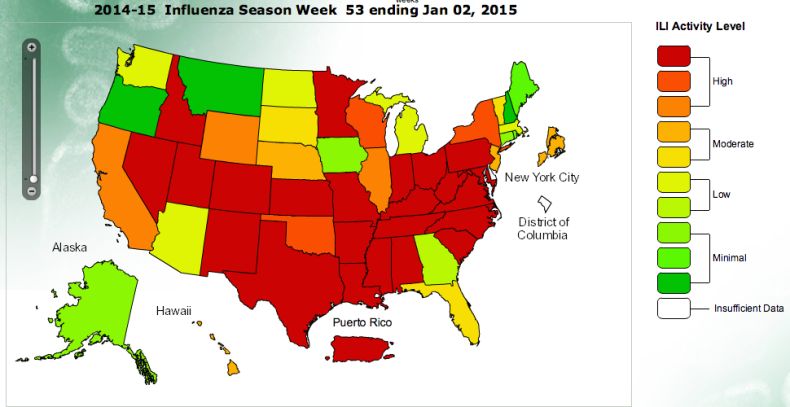
I’d love to see flu activity as a function of locale compared to this vaccination map.
Jennie, CDC doesn’t quite have what you’re looking for, but it does have some cool interactive maps. Worth poking around if you’re curious. http://www.cdc.gov/flu/weekly/fluviewinteractive.htm
Does getting a flu shot every year provide some lasting immunity to the various flu strains in subsequent years? I keep thinking of the 1918 pandemic, and of how older people tended to survive because they had been exposed to a similar virus in the past, but younger people had no such protection.