 Lyme disease is a growing scourge. The Centers for Disease Control and Prevention receives about 30,000 reports of the disease each year, but agency says the number of actual diagnoses could be ten times higher.
Lyme disease is a growing scourge. The Centers for Disease Control and Prevention receives about 30,000 reports of the disease each year, but agency says the number of actual diagnoses could be ten times higher.
Once upon a time, we had a safe and effective vaccine to prevent the disease. But this vaccine, called Lymerix, was withdrawn in 2002, just four short years after it was approved. GlaxoSmithKline, the vaccine’s manufacturer, claimed that it pulled Lymerix because of poor sales, but it’s also true that the company was mired in lawsuits alleging that the vaccine caused serious side effects. In this month’s issue of Nature Medicine, I dive deep into the controversial history of that vaccine and explore how its withdrawal has impacted development of a new vaccine. But that piece focuses on vaccines designed for humans. Today I want to look at another type of Lyme vaccine, one designed for mice.
The demise of Lymerix was a blow to many, including Maria Gomes-Solecki, then a researcher at Stony Brook University. She had been working on a similar vaccine, but after Lymerix tanked, she knew that further research would be fruitless. “Everybody in the field knew that it was going to be very difficult to salvage after this situation,” she says.
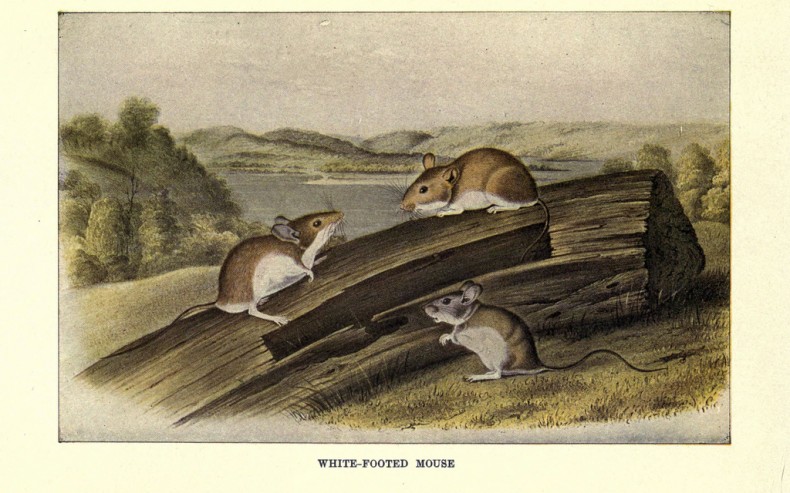
Gomes-Solecki didn’t want all of her hard work to go to waste, so she racked her brain for another application. If she couldn’t use her vaccine on humans, she would use it on mice. People tend to associate Lyme disease with deer because they provide food for adult ticks. But it’s the young ticks that contract the Lyme-causing bacterium, Borrelia burgdorferi. And these little guys feed on mice — the white-footed mouse, primarily.
Gomes-Solecki hoped that by vaccinating mice, she could reduce the number of infected ticks. But not in the way you might think: The mice would receive the vaccine, but the real action would happen in the belly of the tick. Both Lymerix and the vaccine that Gomes-Solecki had been working on contain a protein called OspA. When injected these vaccines prompt the immune system to churn out OspA antibodies. When a tick begins to feed, it takes in a mouthful of antibody-laced blood and rids itself of a bellyful of bacteria. These antibodies protect uninfected mice from becoming infected, but they also help stop infected mice from transmitting the bacterium to ticks.
Gomes-Solecki had an ingenious mechanism, but she still had to come up with a way to deliver the OspA. Vaccinating mice is no easy feat. You can’t convince rodents to line up at a clinic, and injecting mice in the wild would require a massive dragnet. “You can’t go out there and catch every single mouse or little rodent and vaccinate them subcutaneously,” Gomes-Solecki says. What she needed, she decided, was bait — a tasty oral vaccine that mice would willingly devour. The idea wasn’t entirely novel. The USDA had already approved an oral rabies vaccine for raccoons.
Gomes-Solecki spent the next decade developing her vaccine. By 2006 she had formulated oatmeal pellets laced with OspA. Those pellets reduced the number of infected ticks lab studies, and research published earlier this year shows they can also be effective in the field. Gomes-Solecki and her colleagues selected seven football-field-sized plots in Dutchess County, New York and planted them with live traps. Traps on four of the plots were laced with OspA vaccine. The other three plots contained only placebo pellets. By the second year, the vaccine had slashed number of infected ticks by 23%. By the fifth year, the researchers saw a 76% reduction. White-footed mice live about a year, and ticks live about two. So with each passing year, “you keep on taking more and more bacteria out of the ticks,” Gomes-Solecki says.
Whether this strategy could work in the real world, outside the confines of a carefully controlled study, remains to be seen. In the real world, no one would be trapping the mice. The pellets would likely be scattered on the ground or placed in walk-through containers in Lyme disease hotspots. Last year a team of Swiss and American researchers conducted a modeling study to assess the effectiveness of oral vaccination. The scientists found that the dual mode of action creates a positive feedback loop that reduces B. burgdorferi prevalence, and that oral vaccination of mice could be a promising long-term strategy for reducing human Lyme risk.
Still, it’s not a simple strategy, certainly not as simple as vaccinating humans. But Gomes-Solecki doesn’t see another human vaccine coming anytime soon. Pharmaceutical companies are too worried about lawsuits, and the anti-vaccination movement is still going strong. “We have infectious disease bouncing back in the states because people stopped vaccinating their kids for disease that will kill,” she says.
Even if there were a human vaccine available, that wouldn’t make a mouse vaccine obsolete, she points out. “You don’t have a magic solution out there,” she says. “The best situation is an integrated approach.”
Image credit: Biodiversity Heritage Library via Flickr