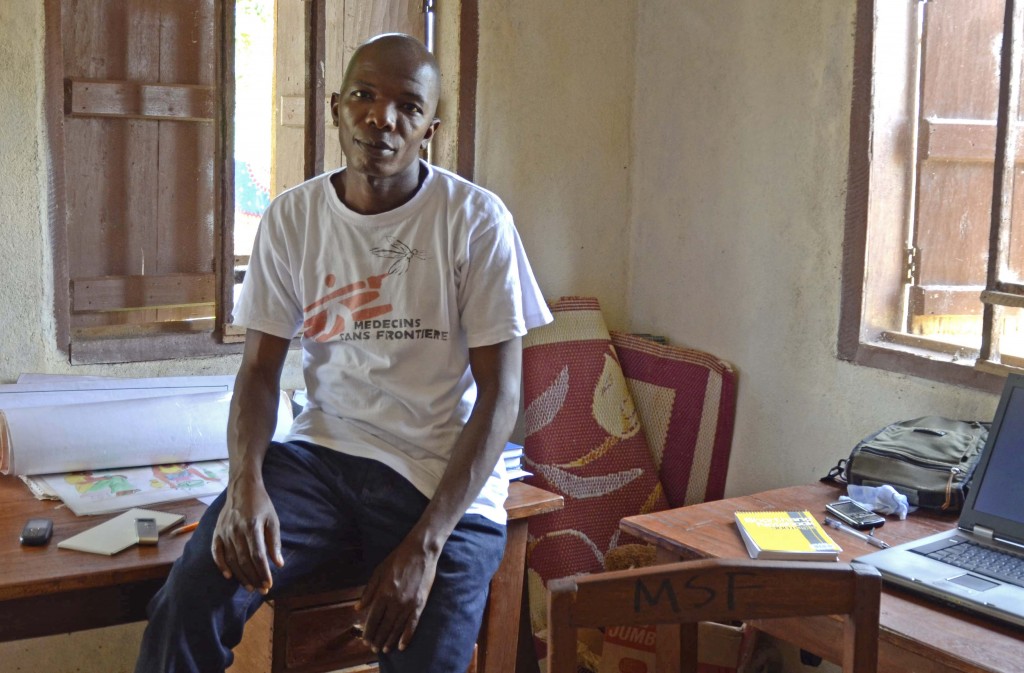
Last November, I spent the hottest hours of a West African afternoon camped outside Tamba Aruna’s office. He’s a slight, soft-spoken man who listens to the sorrows of others each day. His job – mental health supervisor at the emergency clinic operated by Doctors without Borders (or MSF) in Sierra Leone – makes Aruna a hard man to catch. When he found me at his office, he told me the latest. An eight-year-old had signs of Lassa Fever, a potentially lethal hemorrhagic disease that can spread from person-to-person through various bloody excretions. Aruna had been comforting the patient’s mother, and asking her to leave her child at the hospital until the results from the diagnostic test for Lassa returned from a laboratory in a neighboring town. The mother refused. Aruna leaned back against his wooden office desk and said softly, “These are the difficulties.”
At the hospital, Aruna comforts mothers distraught over the loss of the their babies. He speaks with cancer and diabetes patients who are told that treatments for these chronic diseases don’t exist in Sierra Leone, and he advises them on ways to live out their final days. Aruna also prepares physically and sexually abused women and children to return to the community without shame. The MSF clinic is strictly for emergencies, and Aruna says he regrets that he cannot counsel patients for longer. But again, these are the difficulties in a country near the bottom of the United Nations’ development index based on measures like poverty, life expectancy and education.
Whenever public health experts noted a lack of mental health care in developing countries, my assumption was that there were too few psychiatrists to treat the same problems that we face in industrialized countries, like depression, autism and attention deficit disorders. That’s right, but talking to Aruna, I realize the problem is so much worse than I imagined. According to several studies, poverty increases a person’s risk of mental illness because of the chronic stress it induces though a lack of food, medical care, employment and empowerment. It’s also true that impoverished individuals with mental health issues rarely escape poverty. Combine this cycle with the psychological toll of war, and Sierra Leone’s gap in mental health care is disturbingly enormous. Amidst a population of six million, most of whom have endured trauma and live on $2 per day, there is but one permanent psychiatrist located at the one psychiatric ward in Sierra Leone.
Civil war ravaged Sierra Leone between1991 and 2002. Rebel forces traded diamonds for weapons and captured cities by killing, raping, or amputating the limbs of civilians. Children abducted by the rebels were trained in violence. Almost half of the girl combatants have since admitted to being raped by their captors as well. Every Sierra Leonean teen and adult has directly experienced the violence of this “blood diamond” war. For example, a medical professor I met in the capital city of Freetown said that during the war, some of his former students stormed his laboratory. He was out of town, so the students murdered his technicians and stole lab equipment.
Now that the war is over, former combatants live beside victims in tense peace. Outsiders working in Sierra Leone casually toss around the idea that the entire nation suffers from post-traumatic stress disorder. I’m not sure if that’s true. No psychiatrist is available to make the diagnosis.
During the war, Aruna and his brother fled to a refugee camp in neighboring Guinea. There, aid workers from the non-profit organization Center for Victims of Torture recruited Aruna to counsel his distraught countrymen. (The term mental health is laden with stigma throughout Africa, so I’ve adopted their chosen term, counsel.) When Aruna returned to Sierra Leone, he studied “psychosocial counseling” at a college in Freetown. In 2005, MSF hired him to work with Liberians who had fled to a refugee camp in eastern Sierra Leone where the MSF clinic now resides. “Liberian patients were coming to the hospital and complaining of health problems when there was nothing wrong,” Aruna said. Their pain festered deep below the surface.
It’s not hard to understand why aid organizations recruited him. Aruna smiles slightly as he talks, and leaves long pauses after every sentence as if inviting time for reflection. He had several serious crises to attend to that afternoon, but he behaved as if the conversation could last forever if I needed it to. I kept thinking, how does this man not crack?
Aruna admits that he’d like help. In fact, he’s asked for it. He says a female counselor might better reach abused women and girls. Rapists are rarely prosecuted in Sierra Leone, and instead it’s the victims that society may reject. Aruna said about eight sexually abused children end up at the small MSF emergency clinic each month. Staff from larger hospitals put that number closer to forty. “We think the rates are even higher than what hospitals record,” Aruna added. “Many people will never come to the hospital because of the stigmatization they feel.”
Aruna counsels abused children for the few days they stay at the clinic. “I’ll ask them to remember what happened, or to draw what happened,” he said. “I’ll ask if they are afraid to go home or if they feel betrayed …I’ll talk with the mother about how to re-integrate the child into the community, how to protect them and how to get over stigma,” of rape. Abuse tends to plague orphans and children from the most impoverished homes, he said, children who are unlikely to get retribution.

Last week, Aruna emailed me to say that MSF is unlikely to hire another counselor because of budgetary constraints. Salaried mental health positions in Sierra Leone are exceedingly rare, even at aid organizations. For that reason, few Sierra Leonean students study mental health even though they may be best qualified to help. Sierra Leone’s national budget for mental health is negligible. According to blogs, patients are sometimes chained to their beds at the psychiatric ward in Freetown because the hospital does not have the funds to pay for an adequate number of nurses to watch over them. For sake of comparison, the US – a country far from perfect in its record on psychiatric care – spent $135 billion on mental health in 2005.
Aruna also emailed me his notes from a recent meeting organized by the Mental Health Coalition of Sierra Leone. The coalition’s deputy, Gladys Palma, announced that “mental health for all” had been added to the President’s agenda. It’s hard to feel excited. In my two-week visit to Sierra Leone, new political promises captured newspaper headlines daily. Instead, hope comes in the form of Aruna, a man seemingly capable of absorbing people’s pain so that they carry lighter loads. “I always try to see if there’s anything I can do for patients,” he told me. “But mainly, I just listen.”
****
Amy Maxmen is a freelance science journalist who writes about medicine, health, neuroscience, and evolution for a outlets that include Nature, The Scientist, Science News, Psychology Today, Cell and the Lancet. Prior to writing, she earned a Ph.D. from Harvard University by spending a great deal of time in the ocean and beside a microscope in Honolulu.
Photos by Amy Maxmen
An important and disturbing story. Kudos to Aruna, and to you, Amy, for writing this.
You’ve got an inmpressive VITA, Amy. I wish I’d met you 45 years ago…or so.
Alan Plum, Ph.D